While the incidence of non-Hodgkin's lymphoma (NHL) has declined ~1% per year (Y) since 2015, it is not known if this trend holds true for mantle cell lymphoma (MCL). The Surveillance, Epidemiology and End Results (SEER) 17 database includes MCL data collected from 12 US states between 2000 and 2013. However, since the launch of the new SEER 22 database, there has not yet been a study analyzing MCL trends. SEER 22 added seven more years of follow up (up to 2020) compared to SEER 17 (up to 2013), as well as the states of Illinois, Texas, Idaho, Massachusetts, and New York to the 12 states of SEER 17. Here we provide updated trends in MCL incidence and survival using the SEER 22 database, with subset analysis of age, race, and gender.
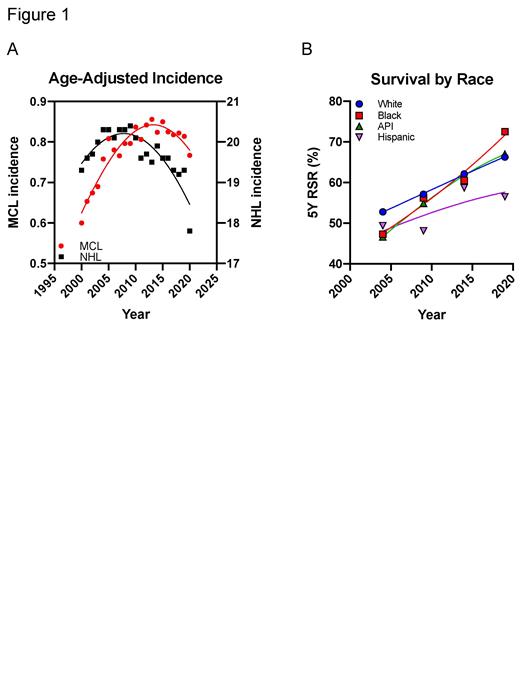
Age-adjusted incidence (per 100,000 Persons/Y) of reported MCL cases were extracted from SEER 22 and tabulated at 5Y intervals (2000-2019). We found an initial increase in MCL incidence from 0.675 (2000-2004) to 0.789 (2005-2009) to 0.833 (2010-2014), followed by a slight decrease to 0.826 (2015-2019) (Fig. 1A). Using the SEER*Stat platform, we calculated the Annual Percent Change (APC) of MCL incidence from 2000 to 2019. The APC is a standard way to statistically characterize trends in MCL rates over time assuming the rates are to change at a constant percentage of the rate of the previous year. While the MCL APC from 2000 to 2014 was +2.02% signaling an annual increase, that for the years 2015 to 2019 was -0.49% indicating an average 0.49% annual decline in MCL incidence since 2015. This decline was found to be statistically significant when compared the 2000-2014 APC.
Unsurprisingly, the incidence of MCL in 2020, the first year of the COVID-19 pandemic, declined to 0.767 compared to 0.814 in 2019, translating into a -5.77% percent change (PC). The PC was calculated as follows: PC=100 x [rate (2020)/rate (2019)-1]. This decrease in MCL rate is less pronounced than the -7.76% PC in NHL incidence in 2020. While these remarkable PCs reflect a drop in reporting and delayed/postponed diagnosis during the first year of the pandemic, the MCL incidence is expected to be less affected considering the aggressive nature of this disease prompting immediate diagnosis and medical care. Notably, the PC in diffuse large B-cell lymphoma (DLBCL) incidence in 2020 compared to 2019 was -3.77%, which contrasts with a larger PC of -8.69% in follicular lymphoma (FL). While DLBCL is aggressive and warrants immediate attention, FL is indolent, and diagnosis tended to be postponed during the early months of the pandemic. Collectively, the observed decrease in MCL incidence in 2020 could potentially reflect a real trend in the continuous MCL decline over time. When we included the 2020 data in the APC analysis, the 2014-2020 APC further decreased to -0.89% compared to -0.49% (2014-2019).
The initial increase in MCL incidence (2000-2014) can be explained by improved reporting (access to electronic medical records, MCL being reported as MCL rather than NHL) and improved diagnostic identification of MCL (SOX11, CD5-negative MCL, indolent MCL, adoption of colonoscopy leading to early MCL detection). Following the observed peak in 2014, MCL incidence seems to follow the overall NHL downward trend.
Subset analysis of age, gender, and race will be included in the presentation. Overall, we observed no major trends, except for an uptrend in the MCL incidence in the Black population potentially reflecting improved access to healthcare.
To compare trends in MCL survival, we analyzed the 5Y observed overall survival (OS). Additionally, we calculated the relative survival rate (RSR) as the ratio of the observed OS divided by the expected OS of an age-matched comparable group from the general population. The 5Y observed OS improved over time: 45.2% (2000-2004), 49.1% (2005-2009), 53.8% (2010-2014), and 57.1% (2015-2019). This translated in a marked improvement in the 5Y RSR reaching 65.5% in 2015-2019. Unfortunately, while the 5Y RSR of the Hispanic population improved over time, it continues to be significantly lower than the non-Hispanic populations, reflecting either a disparity in access to healthcare or an overall worse prognosis. This dramatically contrasts with the 5Y RSR of the Black population, which once was among the lowest (47.3%, 2000-2004), became the highest 72.5%, (2015-2019) reflecting not only a better access to healthcare, but also a shift to a previously unrecognized better overall prognosis of MCL in Black patients (Fig. 1B).
Disclosures
Saba:Seagen: Consultancy, Research Funding; AbbVie: Consultancy, Honoraria, Speakers Bureau; ADC Therapeutics: Consultancy; Janssen Biotech: Consultancy, Honoraria, Speakers Bureau; Eli Lilly: Consultancy; Incyte Corporation: Consultancy, Research Funding; Genentech USA: Consultancy; BeiGene USA: Consultancy, Speakers Bureau; Merck: Research Funding; MorphoSys: Research Funding; Acerta: Research Funding; Karyopharm Therapeutics: Research Funding; AstraZeneca: Research Funding; Amgen: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal